Overview
Between February and December 2025, the Community Pot Nutrition Stabilization Centre (NSC) pilot was implemented in Ibadan North-West Local Government Area, Oyo State, as a community-based intervention to address acute malnutrition among children aged 6–59 months.
The pilot focused on early detection of malnutrition, caregiver counselling, community nutrition education, and referral linkages with health facilities. This page presents a summary of outcomes, insights, and recommendations from the pilot phase.
National nutrition evidence from the National Food Consumption and Micronutrient Survey (NFCMS) provides important context for this work. The NFCMS reports that in the South-West zone, approximately 6–7% of children under five experience wasting, around 30% are stunted, and 18–20% are underweight. These population-level findings highlight the presence of both acute and chronic malnutrition risks in the region, even when they are not always visible at household level.
Program Objectives
1. Screen children aged 6–59 months regularly to detect moderate and severe acute malnutrition (MAM/SAM).
2. Counsel caregivers of malnourished children through personalised home visits and support sessions.
3. Educate communities on optimal feeding, hygiene, and childcare practices to prevent malnutrition.
4. Strengthen collaboration with local health authorities and community groups to improve referral and continuity of care.
Key Findings
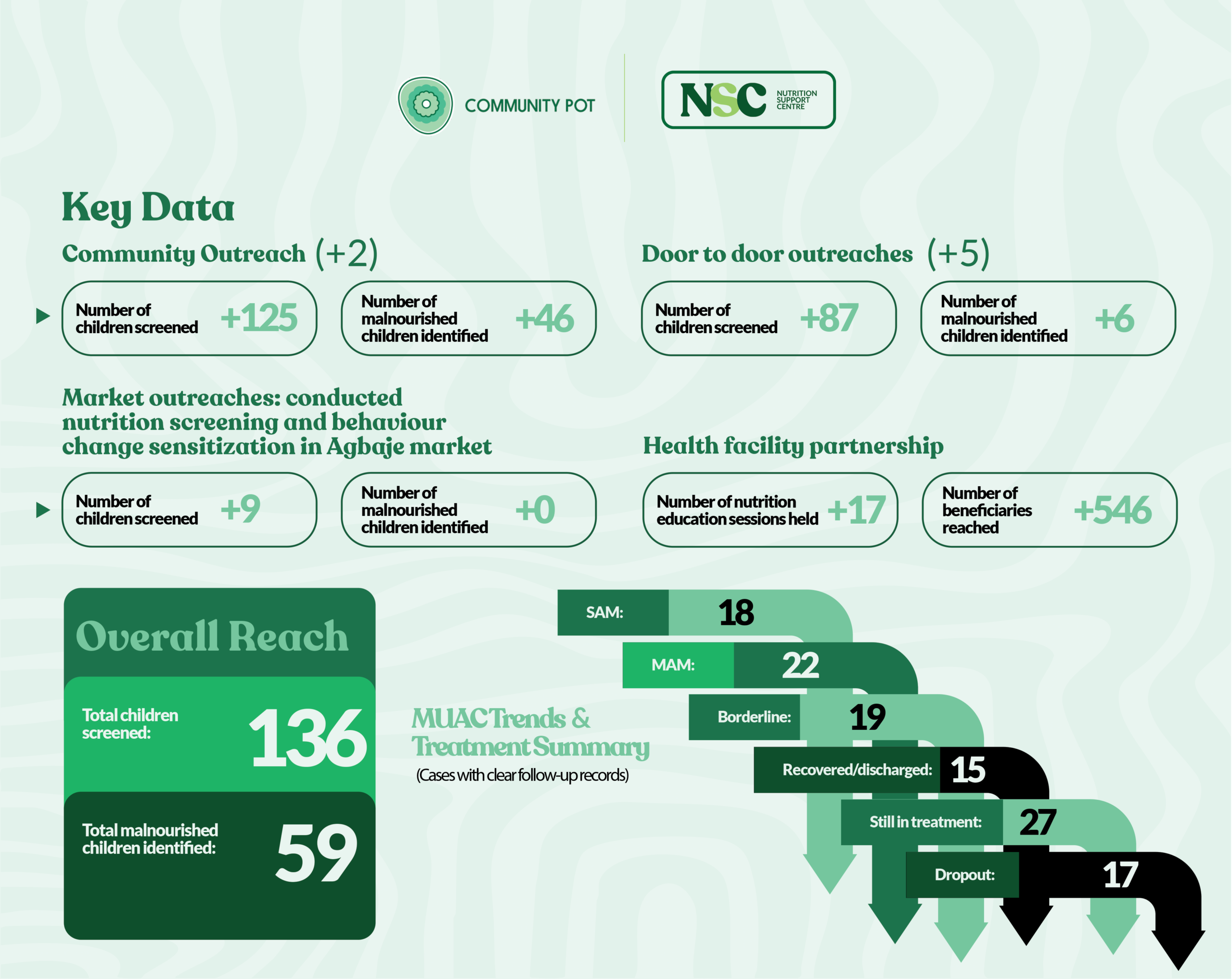
Screening & Coverage
● Total children screened: 136
● Target age group: 6–59 months
● Estimated population coverage: ~90% of target communities
While national surveys estimate malnutrition prevalence at population level, the NSC pilot focused on targeted MUAC screening within high-risk communities. This approach enabled the identification of children who may not be captured through population averages but require immediate support and follow-up.
Malnutrition Burden Identified
● Total malnourished children identified: 59 (43.4%)
○ Severe Acute Malnutrition (SAM): 18
○ Moderate Acute Malnutrition (MAM): 22
○ Borderline MUAC cases: 19
All identified cases were enrolled for follow-up and support.
The proportion of malnourished children identified through the NSC pilot reflects the concentration of nutrition risk within targeted communities. Unlike national surveys, which estimate prevalence across broad populations using anthropometry, community-level MUAC screening is designed to identify acute cases among children actively reached by services. These figures therefore represent case burden rather than population prevalence.
Treatment Outcomes
● Recovered and discharged: 15 children (25.4%)
● Still in active treatment: 27 children (45.8%)
● Defaulted before completion of care: 17 children (28.8%)
Caregiver compliance with follow-up visits was low, with only 8.5% demonstrating good adherence.
Behavioural and Care Practice Improvements
Despite follow-up challenges, notable positive changes were observed:
● 100% increase in reported meal frequency among enrolled households
● Continued breastfeeding among 50% of children
● Increased caregiver interest in complementary feeding practices
● Observable improvements in child energy levels at endline
Geographic variation was observed, with better retention and follow-up compliance in settlements supported by active community mobilisers.
These behavioural improvements are consistent with broader evidence that inadequate dietary diversity and protein intake contribute significantly to child nutrition challenges. National findings indicate low dietary diversity among young children in the South-West zone, reinforcing the importance of caregiver education and early intervention alongside treatment.
Community and Volunteer Engagement
● Total community volunteers mobilised: 90
● Volunteers active throughout implementation: ~53%
Volunteers supported screening, caregiver counselling, follow-up, and data collection, contributing to broad coverage, improved data quality, and increased community acceptance of the intervention.
Implementation Activities Summary
Community Outreach
● Outreach events conducted: 2
● Children screened: 125
● Malnourished children identified: 46
Door-to-Door Outreach
● Door-to-door outreaches conducted: 5
● Children screened: 87
● Malnourished children identified: 6
Market Outreach (Agbaje Market)
● Children screened: 9
● Malnourished children identified: 0
● Activities included nutrition screening and behaviour change sensitisation
Health Facility Partnerships
Behaviour Change Communication (BCC) sessions were conducted in partner health facilities covering breastfeeding, complementary feeding, hygiene practices, food diversification, and malnutrition prevention.
● Nutrition education sessions held: 17
● Total beneficiaries reached: 546
Nutrition assessments were also conducted, with malnourished children referred to the NSC kiosk for follow-up care.
Embedding services within health facilities enabled NSC to align with routine immunisation and antenatal care platforms, increasing reach and trust. This approach complements national health system efforts by translating population-level nutrition evidence into targeted community action.
MUAC Trends and Treatment Summary
(Cases with clear follow-up records)
● Children followed up: 59
● SAM cases: 18
● MAM cases: 22
● Borderline MUAC cases: 19
● Recovered and discharged: 15
● Still in treatment: 27
● Dropout rate: 17 children (28.8%)
Key Challenges Identified
● Distance to service points limiting caregiver access
● Caregiver work and time constraints
● Perceived child improvement leading to early discontinuation of care
● Limited decentralised community-based follow-up points
Recommendations
Strengthen Follow-Up and Retention
● Introduce proactive tracking for missed appointments through home visits and phone reminders
● Assign community-based case managers to reduce default rates
Decentralise Service Delivery
● Expand mobile and community-based follow-up points to reduce distance and access barriers
Sustain Community Sensitisation
● Maintain periodic nutrition education sessions and mother-to-mother support activities
● Reinforce early care-seeking and optimal feeding practices
Formalise Referral Linkages
● Strengthen integration with Primary Health Centres (PHCs) and LGA health services
● Improve continuity of care for complicated SAM cases
Improve Data Quality
● Implement routine data checks at each contact point
● Continue digitisation